MRCPUK SEND Endocrinology and Diabetes (Specialty Certificate Examination) Online Training
MRCPUK SEND Online Training
The questions for SEND were last updated at Dec 13,2025.
- Exam Code: SEND
- Exam Name: Endocrinology and Diabetes (Specialty Certificate Examination)
- Certification Provider: MRCPUK
- Latest update: Dec 13,2025
A 72-year-old man with a dense residual hemiparesis and unsafe swallow was fed via a percutaneous gastrostomy for 20 hours each day. He had type 2 diabetes mellitus that had been well controlled with metformin.
His glucose levels were uncontrolled on metformin powder at maximum dose.
According to the Joint British Diabetes Societies Guidelines (2012), what is the most appropriate next hypoglycaemic agent?
- A . exenatide
- B . gliclazide
- C . insulin detemir
- D . insulin glargine
- E . premixed (30/70) human insulin
A 23-year-old barmaid presented with headache, sweating and collapse. She had a past medical history of tension headache and unexplained abdominal pain. Her regular medication included amitriptyline 25 mg at night and paracetamol 1 g as required. She was a smoker and regularly drank alcohol.
On examination, her pulse was 120 beats per minute and her blood pressure was 210/128 mmHg.
Investigations:
24-h urinary metanephrine5.4 µmol (<2)
24-h urinary normetanephrine15.2 µmol (<3)
What substance is most likely to cause assay interference in the measurement of urinary metanephrines?
- A . alcohol
- B . amitriptyline
- C . caffeine
- D . nicotine
- E . paracetamol
A 16-year-old Caucasian girl presented with a 4-year history of facial hair growth, acne and secondary amenorrhoea.
On examination, her body mass index was 20 kg/m2 (18C25). Her gums and palmar creases were pigmented. Facial hair was evident on her upper lip and chin, and terminal hair was evident on her chest and abdomen. Her FerrimanCGallwey score was 25. She had acne affecting her face and back.
Investigations:
serum dehydroepiandrosterone sulphate15 µmol/L (3C12)
serum androstenedione12.2 nmol/L (0.6C8.8)
serum 17-hydroxyprogesterone120 nmol/L (1C10)
serum testosterone6.0 nmol/L (0.5C3.0)
serum sex hormone binding globulin18 nmol/L (40C137)
What treatment is likely to be of most benefit?
- A . cyproterone acetate
- B . fludrocortisone
- C . flutamide
- D . hydrocortisone
- E . metformin
A 26-year-old physiologist was seen in the diabetes outpatient clinic. She had type 1 diabetes mellitus of 9 months’ duration, treated with subcutaneous insulin.
She asked what symptoms of hypoglycaemia she might experience.
In what order are responses to hypoglycaemia most likely to occur as blood glucose falls?
- A . autonomic, counter-regulatory hormones, neuroglycopenia
- B . autonomic, neuroglycopenia, counter-regulatory hormones
- C . counter-regulatory hormones, autonomic, neuroglycopenia
- D . counter-regulatory hormones, neuroglycopenia, autonomic
- E . neuroglycopenia, autonomic, counter-regulatory hormones
A 56-year-old man attended routine follow-up for treatment of hypogonadism of late onset. His only medication was testosterone undecanoate (1 g intramuscular injection, every 12 weeks). He had started this treatment 12 months previously and last received the injection 1 week before review.
Digital rectal examination was normal.
Investigations (baseline):
haemoglobin145 g/L (130C180)
haematocrit0.46 (0.40C0.52)
serum prostate-specific antigen0.6 µg/L (<4)
Investigations (12 months after treatment):
haemoglobin153 g/L (130C180)
haematocrit0.51 (0.40C0.52)
serum prostate-specific antigen5.1 µg/L (<4)
What is the most appropriate next step in management?
- A . check serum testosterone
- B . decrease testosterone injection frequency to 14 weeks
- C . reassure and repeat blood tests in 12 months
- D . refer for urological assessment
- E . stop testosterone therapy
An 18-year-old woman was referred by her general practitioner for further investigation of “funny turns” during which she developed palpitations, sweating, tremor, hunger, anxiety and paraesthesiae; all of these symptoms were relieved immediately by a sugary drink.
She was otherwise well and was not taking any regular medication. There was a family history of type 1 diabetes mellitus. A spontaneous hypoglycaemic episode had not been captured and she was admitted to the diabetes/endocrine ward for a 72-hour fast. Her renal function was normal.
After a 12-hour fast she experienced her typical symptoms. Urinalysis showed no urinary ketones.
Investigations after 12-h fast:
fasting plasma glucose 2.0 mmol/L (3.0C6.0)
plasma insulin56 pmol/L (<21 after hypoglycaemia)
serum C-peptide514 pmol/L (180C360)
What is the most appropriate next step in management?
- A . coeliac axis angiography
- B . MR scan of abdomen and pelvis to localise a mesenchymal tumour producing insulin-like growth factor 2
- C . MR scan of pancreas to localise an insulinoma
- D . obtain a careful history looking for access to exogenous insulin
- E . request a urinary sulphonylurea screen on sample obtained during the fast
A 32-year-old man presented with medullary thyroid cancer, treated by total thyroidectomy. He had a past history of primary hyperparathyroidism, treated by selective parathyroidectomy. Postoperatively, plasma calcitonin was undetectable and serum calcium was in the normal range.
Investigations:
RET genotypeheterozygote codon 634 C>T mutation
What is the most appropriate approach to annual screening for phaeochromocytoma?
- A . biochemical screening
- B . CT scan of adrenal glands
- C . MIBG scanning
- D . MR scan of adrenal glands
- E . octreotide scanning
A 54-year-old woman was referred for assessment of low bone mineral density. Three months previously, after complaining of bloating and flatulence, she had been found to have coeliac disease and had been started on a gluten-free diet. She had no history of fracture and had not lost height. There was no family history of osteoporosis. Her only medication was omeprazole.
Investigations:
serum corrected calcium2.42 mmol/L (2.20C2.60)
serum alkaline phosphatase122 U/L (45C105)
plasma parathyroid hormone7.9 pmol/L (0.9C5.4)
DXA scansee image
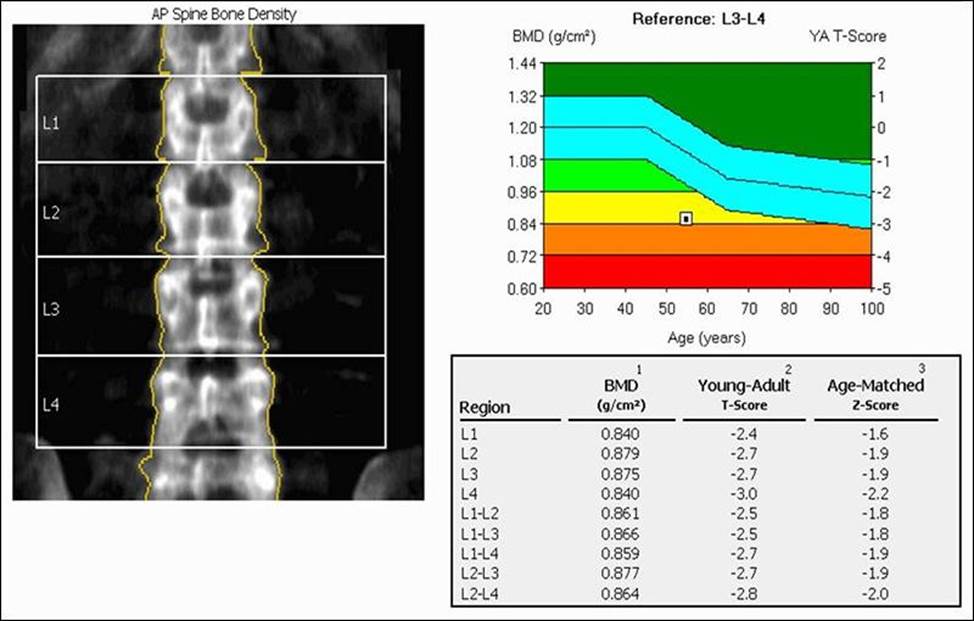
What is the most appropriate treatment?
- A . alendronic acid alone
- B . alendronic acid, and calcium and vitamin D
- C . calcium and vitamin D
- D . calcium and vitamin D, and intravenous zoledronic acid
- E . strontium ranelate
A 34-year-old woman with Addison’s disease reported four adrenal crises over the preceding 6 months, requiring hospital admission and intravenous administration of hydrocortisone. At outpatient follow-up, she was taking hydrocortisone 15 mg in the morning and 10 mg at midday, and fludrocortisone 50 micrograms daily.
What is the most important next step in management to prevent further crises?
- A . change to sustained-release hydrocortisone
- B . increase dosage of hydrocortisone
- C . measure plasma adrenocorticotropic hormone
- D . measure plasma renin
- E . measure post-dose 09.00 h cortisol
A 55-year-old dental nurse was referred for bone densitometry after sustaining a non-displaced fracture of the femur after falling down a step. She had experienced no other fractures. Her only medical problem was long-standing anaemia of unknown cause. The only family history was of persistent dental abscesses affecting her father. She had three children who were well. She was taking no medication.
Examination was normal.
Investigations:
haemoglobin102 g/L (115C165)
MCV85 fL (80C96)
white cell count6.0 ? 109/L (4.0C11.0)
platelet count245 ? 109/L (150C400)
erythrocyte sedimentation rate25 mm/1st h (<30)
serum creatinine85 µmol/L (60C110)
serum corrected calcium2.40 mmol/L (2.20C2.60)
serum alkaline phosphatase56 U/L (45C105)
DXA scan spine (L2CL4)T score +5.8
DXA scan total hipT score +5.4
What is the most likely diagnosis?
- A . fluorosis
- B . high bone mass phenotype
- C . myelodysplasia
- D . osteopetrosis
- E . Paget’s disease
Latest SEND Dumps Valid Version with 200 Q&As
Latest And Valid Q&A | Instant Download | Once Fail, Full Refund

