How many cases are left?
Topic 1, Humongous Insurance
Case Study
This is a case study. Case studies are not timed separately. You can use as much exam time as you would like to complete each case. However, there may be additional case studies and sections on this exam. You must manage your time to ensure that you are able to complete all questions included on this exam in the time provided.
To answer the questions included in a case study, you will need to reference information that is provided in the case study. Case studies might contain exhibits and other resources that provide more information about the scenario that is described in the case study. Each question is independent of the other questions in this case study.
At the end of this case study, a review screen will appear. This screen allows you to review your answers and to make changes before you move to the next section of the exam. After you begin a new section, you cannot return to this section.
To start the case study
To display the first question in this case study, click the Next button. Use the buttons in the left pane to explore the content of the case study before you answer the questions. Clicking these buttons displays information such as business requirements, existing environment, and problem statements. If the case study has an All Information tab, note that the information displayed is identical to the information displayed on the subsequent tabs. When you are ready to answer a question, click the Question button to return to the question.
Background
Humongous Insurance is contracted to process all insurance claims for a health facility that accepts the following types of health insurance:
✑ Health maintenance organization (HMO)
✑ Preferred-provider organization (PPO)
✑ Gold
Cases are classified as new claims, claim disputes, and follow-ups. Each insured person is entitled to open 25 new cases each calendar year.
Support representatives specialize by and process claims by insurance type.
Humongous Insurance currently accepts claims only by telephone. The call center is open from 06:00 GMT to 24:00 GMT daily. Call center staff work one of the following shifts: 06:00 GMT to 12:00 GMT, 12:00 GMT to 18:00 GMT, and 18:00 GMT to 24:00 GMT.
When a case is received by email, a staff member categorizes the case as email and closes the case immediately.
Current environment
✑ Humongous Insurance has three departments to handle claim types: HMO, PPO, and Gold.
✑ The company uses handwritten forms to send claims information to the correct department.
✑ Each department maintains a workbook to record calls received.
Requirements. Support desk
✑ Configure the system to track the number of insurance claims filed each year.
✑ Categorize claims by type as they are opened.
✑ Configure the system to track staff responsiveness to service-level agreements (SLAs).
✑ Ensure that business hours reflect the hours that support staff are scheduled.
Requirements. Case handling
✑ All new cases must be automatically placed into a queue based on insurance type after the type is selected.
✑ All insurance types need to be automatically moved to the proper queue when the subject is picked.
✑ All cases must be created and closed immediately when received.
✑ The status reason must be set to Email Sent or Phone Call.
✑ Information must be restricted by insurance and phone call type.
✑ Managers must be alerted when customers reach their limit of 25 cases for the year.
✑ Changes to cases must not be counted against entitlements until the case is closed.
Requirements. Disputes
✑ Claim disputes must be categorized as low priority.
✑ The status for all disputed cases must be set to Review by a Manager before a disputed case may be closed.
Requirements. Knowledge base
✑ A knowledge base must be used as a repository for all answers.
✑ Representatives must be able to search the knowledge base when opening a new case for similar claims.
✑ Representatives must be able to search across all entities at all times.
✑ Searches must check any field in the entity for matches in a single search.
✑ Searches must return results in a single list and sort the list so that the most relevant results appear at the top of the list.
✑ Representatives must be able to link the knowledge base to cases when applicable.
✑ Representatives must create a new knowledge base article if an answer is not found in the existing knowledge base.
✑ Representatives must be able to use SQL-like syntax to search the knowledge base.
Requirements. Service-level agreements
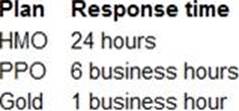
When a customer calls to open a claim, the company must respond to the caller within the following time frames:
Requirements. Alerts
✑ Cases must be flagged when they are past the SLA threshold.
✑ An email alert must be sent to the manager to indicate an SLA noncompliance.
✑ An email alert must be sent to representatives for SLA violations as follows: HMO 2 hours prior and PPO 1 hour prior.
✑ Send an email alert to support managers when disputes are ready to be closed.
✑ Send an email alert to customers when cases are closed.
Requirements. Issues
✑ The current process is all manual and not efficient.
✑ There is no easy way to determine whether the company is meeting its SLAs.
✑ Representatives are often inconsistent regarding how they handle customers and answer customer questions.
✑ There is no accountability for any of the representatives who take calls.
A customer has three cases in process and two cases for the current calendar year.
You need to determine how many cases the customer has left on their entitlement.
How many cases are left?
A . 20
B. 22
C. 23
D. 25
Answer: C
Explanation:
Reference: https://docs.microsoft.com/en-us/dynamics365/customer-service/create-entitlement-define-support-termscustomer
Latest MB-230 Dumps Valid Version with 105 Q&As
Latest And Valid Q&A | Instant Download | Once Fail, Full Refund

